Solutions
Scalable RCM solutions boosting revenue, efficiency, outcomes, and satisfaction.

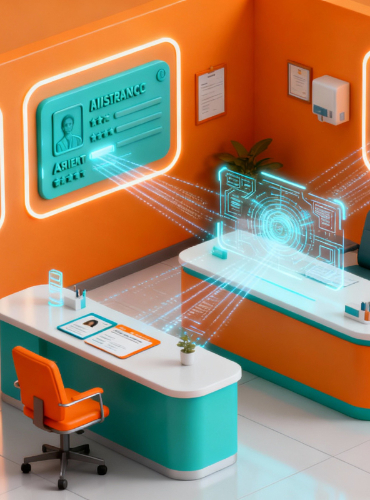
1. End-to-End Revenue Cycle Management
EIQ Healthcare LLP is your dependable, all-in-one partner for complete end-to-end Revenue Cycle Management. We ensure precise eligibility and benefits verification, followed by clean claim submission and proactive tracking to accelerate reimbursements and reduce operational burdens.
Our team handles payment posting and reconciliation with exceptional accuracy, while driving consistent AR follow-up to minimize delays and strengthen denial management. To support informed decision-making, we provide comprehensive financial reporting and analytics that reveal performance trends, identify bottlenecks, and uncover opportunities for increased revenue.
With EIQ Healthcare LLP, you gain a fully optimized, technology-enabled, and data-driven revenue cycle designed to maximize collections, improve efficiency, and strengthen the financial health of your practice.
2. Accounts Receivable (AR) Management
Our Accounts Receivable (AR) Management service ensures faster recovery and healthier cash flow through focused follow-up on 30/60/90+ day claims. We conduct thorough root-cause analysis of denials to identify patterns and implement corrective actions that prevent recurring issues. By streamlining AR processes, we help significantly reduce Days Sales Outstanding (DSO) and boost overall cash flow efficiency. To ensure a transparent relationship with our clients, EIQ Healthcare LLP team also provides KPI-based reporting along with clear, actionable weekly AR dashboards that highlight performance, trends, and priority accounts.


3. Denial Prevention & Management
Our Denial Prevention & Management service is built to eliminate revenue leakage at its source. We identify recurring denial trends, resolve issues swiftly, and collaborate directly with major U.S. payers—including UnitedHealthcare, Anthem/Blue Cross Blue Shield, Aetna, and Cigna—to ensure claims move seamlessly through the reimbursement cycle.
By implementing strategic front-end improvements, strengthening documentation accuracy, and reinforcing coding compliance, we significantly reduce avoidable denials and elevate your clean-claim success rate. Working with us will help you gain a proactive as well as data-driven team for creating a preventive denial strategy. EIQ Healthcare LLP enhances your cash flow & accelerates collections. Thus, ensuring a strong revenue cycle performance year-round.
4. Credentialing & Provider Enrollment
Our Credentialing & Provider Enrollment service ensures a smooth, accurate, and timely onboarding experience with all major payers. We manage the entire process—from initial application to approval—so providers can begin seeing patients without delays.
Our team handles complete Council for Affordable Quality Healthcare (CAQH) setup, maintenance, and revalidations, ensuring every profile stays current, compliant, and payer-ready. We also monitor application progress in real time, manage renewals proactively, and prevent participation gaps that could disrupt reimbursements.
Believe the team at EIQ Healthcare LLP and let us help you smoothen the process of credentialing. We are your efficient, reliable and fully optimized support system for continuous revenue flow.


5. Prior Authorization & Eligibility
Our Prior Authorization & Eligibility service delivers fast, accurate, and proactive authorization management to prevent treatment delays and revenue loss. We perform comprehensive eligibility and benefits verification through payer portals and EDI tools, ensuring complete clarity on coverage, policy rules, and prior authorization requirements before services are scheduled.
To keep operations running smoothly, we maintain real-time communication with provider teams for quick clarifications, prompt document submission, and immediate status updates. This streamlined, technology-driven approach reduces denials, accelerates approval turnaround times, and creates a more efficient, patient-focused workflow.
6. DME & Specialty Billing
Our DME & Specialty Billing service provides specialized expertise in managing complex documentation, modifiers, and billing codes to ensure every claim is accurate, compliant, and paid on time. We support diverse specialty workflows—including laboratory services, orthopedics, radiology, internal medicine, and other advanced clinical disciplines—delivering billing precision tailored to each practice’s unique requirements.
With deep domain knowledge and meticulous attention to detail, we minimize coding errors, increase clean claim acceptance, and streamline the end-to-end revenue cycle. For providers handling intricate and high-volume specialty billing, EIQ Healthcare LLP ensures consistency, compliance, and stronger financial performance.